Physical Therapy After Bunion And Hammertoe Surgery
 Overview
Overview
What Is A Hammer toe? A hammer toe, or claw toe, describes a condition where the toe(s) become buckled, contracted or crooked. The toe could even cross over an adjacent toe, which is called a cross over toe. Any of the toes may be affected, but the 2nd and 5th toe are most commonly involved.
Causes
Many disorders can affect the joints in the toes, causing pain and preventing the foot from functioning as it should. A mallet toe occurs when the joint at the end of the toe cannot straighten. Excessive rubbing of the mallet toe against the top of the shoe can lead to pain and the development of a corn. The tip of the toe is often turned down against the shoe causing pressure and discomfort. Arthritis can also lead to many forefoot deformities including mallet toes. Mallet toes can cause extreme discomfort, and can be aggravated if restrictive or improperly fitting footwear is worn for a prolonged period of time.
 Symptoms
Symptoms
The most common symptoms of hammertoes include. The toe is bent upward at the middle toe joint, so that the top of this joint rubs against the top of the shoe. The remainder of the toe is bent downward. Pain upon pressure at the top of the bent toe from footwear. The formation of corns on the top of the joint. Redness and swelling at the joint contracture. Restricted or painful motion of the toe joint. Pain in the ball of the foot at the base of the affected toe. This occurs because the contracted digit puts pressure on the metatarsal head creating callouse and pressure on the ball of the foot.
Diagnosis
Your healthcare provider will examine your foot, checking for redness, swelling, corns, and calluses. Your provider will also measure the flexibility of your toes and test how much feeling you have in your toes. You may have blood tests to check for arthritis, diabetes, and infection.
Non Surgical Treatment
Wear sensible shoes. If you don?t want to have surgery to fix your hammertoe, use non-medicated padding along with proper shoes made with a wider and deeper toe box to accommodate your foot?s shape. Ensuring your shoes have a good arch support can slow the progression of the condition as well. Use a pumice stone. The corn or callus that forms on top of the hammertoe can cause discomfort when you wear shoes. Treat the corn by using a file or pumice stone to reduce its size after a warm bath, then apply emollients to keep the area softened and pliable. Use silicone or moleskin padding on top of the area when wearing shoes. Do foot exercises. Theoretically, exercises like extending, then curling the toes, splaying the toes, and moving the toes individually may Hammer toe help prevent the digital contracture that causes hammertoe. Try these suggestions and see what works best for you.
Surgical Treatment
A variety of anaesthetic techniques are possible. Be sure an discuss this with your surgeon during your pre-op assessment. The type of surgery performed will depend on the problem with your toes and may involve releasing or lengthening tendons, putting joints back into place, straightening a toe and changing the shape of a bone.Your surgeon may fix the toes in place with wires or tiny screws.
Hammertoes Treatment Options
 Overview
Overview
Hammer toes can result in pain and difficulty in moving the toe. Corns, calluses and blisters can occur from the rubbing of the contracted toe against the inside of the footwear. Both Hammer toes and mallet toe can cause pain during walking, running and other activities. If left untreated, the tendons of the toe may contract and tighten, causing the toe to become permanently stiff and contracted. A podiatric physician or surgeon may have hammertoe to cut or realign tendons and/or remove pieces of bone to straighten the toe. This may require that the bones be fixed temporarily with pins while the toe heals.
Causes
Many disorders can affect the joints in the toes, causing pain and preventing the foot from functioning as it should. A mallet toe occurs when the joint at the end of the toe cannot straighten. Excessive rubbing of the mallet toe against the top of the shoe can lead to pain and the development of a corn. The tip of the toe is often turned down against the shoe causing pressure and discomfort. Arthritis can also lead to many forefoot deformities including mallet toes. Mallet toes can cause extreme discomfort, and can be aggravated if restrictive or improperly fitting footwear is worn for a prolonged period of time.
 Symptoms
Symptoms
A hammertoe causes you discomfort when you walk. It can also cause you pain when trying to stretch or move the affected toe or those around it. Hammertoe symptoms may be mild or severe. Mild Symptoms, a toe that is bent downward, corns or calluses. Severe Symptoms, difficulty walking, the inability to flex your foot or wiggle your toes, claw-like toes. See your doctor or podiatrist right away if you develop any of these symptoms.
Diagnosis
First push up on the bottom of the metatarsal head associated with the affected toe and see if the toe straightens out. If it does, then an orthotic could correct the problem, usually with a metatarsal pad. If the toe does not straighten out when the metatarsal head is pushed up, then that indicates that contracture in the capsule and ligaments (capsule contracts because the joint was in the wrong position for too long) of the MTP joint has set in and surgery is required. Orthotics are generally required post-surgically.
Non Surgical Treatment
Hammer toes may be effectively corrected in different ways. Treatments can be non-invasive and involve physical therapy along with the advice that the person not wear any more shoes that restrict appropriate space for their toes. Appropriate shoes for people who want to avoid hammer toes, or for people who already have them, should be at least half an inch longer than the person's longest toe. High-heeled shoes are something to definitely avoid.
Surgical Treatment
Treatment of a severe hammertoe that has become rigid includes surgery. What is done during the surgery depends on how misshapen and inflexible the toe is. The surgeon may make a cut over your toe and release the tendon by cutting the tendon away from the bone. The surgeon may remove a small piece of bone from the toe. The surgeon may realign the tendons to reposition your toe or fasten the bones with pins. Sometimes the surgeon may have to join the bones in the toe. In this case, you will no longer be able to bend the toe, but the toe will be flat.
Bunions Reasons Indicators And Treatment Procedures
Overview
 Hallux abductovalgus (HAV) or bunion, is a commonly seen deformity of the first metatarsophalangeal joint (MPJ) in which the hallux is abducted and everted, frequently overriding the second toe. Although the terms HAV and bunion are often used synonymously (as is done in this paper), it should be noted that a bunion actually refers to the callus and inflamed adventitious bursa overlying the HAV deformity. Even though bunions have been described in the medical literature for several hundred years (the word bunion is believed to be derived from the Latin, bunio, meaning turnip), there continues to be much controversy concerning its etiology. This is most likely because the development of HAV is multifactorial, stemming from a variety of structural and functional aberrancies.
Hallux abductovalgus (HAV) or bunion, is a commonly seen deformity of the first metatarsophalangeal joint (MPJ) in which the hallux is abducted and everted, frequently overriding the second toe. Although the terms HAV and bunion are often used synonymously (as is done in this paper), it should be noted that a bunion actually refers to the callus and inflamed adventitious bursa overlying the HAV deformity. Even though bunions have been described in the medical literature for several hundred years (the word bunion is believed to be derived from the Latin, bunio, meaning turnip), there continues to be much controversy concerning its etiology. This is most likely because the development of HAV is multifactorial, stemming from a variety of structural and functional aberrancies.
Causes
Improper footwear. Podiatric physicians have long believed that narrow, poor-fitting shoes with a tight toe box tend to compress the end of the foot, leading to abnormal motion of the foot and pressure over the MTP joint. High-heeled shoes tend to add even more pressure to the toes, as the foot slides downward. Over time, continued pressure will squeeze the toes together, encouraging the deformity. Occupational hazards. Individuals whose jobs place undue stress on their feet are among those who complain of bunions. Ballet dancers, in particular, put great demands on their toes, and thus are often subject to bunions, however, they are not alone. Many professionals whose jobs require a great deal of standing or walking (teachers, police officers, doctors and nurses, etc.) and/or who are required to wear a particular type of shoe or boot as part of a uniform, also are at risk. Athletes such as runners or walkers, who utilize the wrong footwear, may also develop bunions.
Symptoms
With an advanced bunion, the big toe joint can be significantly deformed. The big toe can crowd the other toes and may lie over or under the second toe. The larger the bunion gets, the more it hurts to walk. Wearing any type of shoe can be painful. Symptoms of bunions tend to increase over time as the condition worsens. Typical symptoms include deformity of the big toe joint. Growth of a bony lump (exostosis) at the side of the big toe joint. Pain, redness and tissue swelling (bursitis) over the big toe joint, with thickening of overlying skin. Pain when walking (particularly during the "push off" phase). Overlapping of the big toe above or below the second toe in severe cases.
Diagnosis
Before examining your foot, the doctor will ask you about the types of shoes you wear and how often you wear them. He or she also will ask if anyone else in your family has had bunions or if you have had any previous injury to the foot. In most cases, your doctor can diagnose a bunion just by examining your foot. During this exam, you will be asked to move your big toe up and down to see if you can move it as much as you should be able to. The doctor also will look for signs of redness and swelling and ask if the area is painful. Your doctor may want to order X-rays of the foot to check for other causes of pain, to determine whether there is significant arthritis and to see if the bones are aligned properly.
Non Surgical Treatment
If you suspect a bunion, it is essential that you confirm your suspicions by consulting with a podiatric physician. Don?t try to treat the problem yourself, even by using conservative measures. Many conditions have similar symptoms, and only a professional can tell the difference. Once a diagnosis is obtained, it is essential to begin treatment immediately. Your podiatric physician will advise you on the most effective means. If caught early enough, good foot care, shoes that fit properly, and/or orthoses may eliminate the need for any further intervention. Certain over-the-counter remedies, such as felt or foam pads, applied to specific areas of the foot to relieve pressure and friction, will protect the bunion. Elevating the foot and icing the area for 20 minutes an hour may help to relieve pain. 
Surgical Treatment
Depending on the size of the enlargement, misalignment of the toe, and pain experienced, conservative treatments may not be adequate to prevent progressive damage from bunions. In these cases, bunion surgery, known as a bunionectomy, may be advised to remove the bunion and realign the toe.
Prevention
To minimize the chance of developing bunions, never force your feet into shoes that don?t fit. Choose a shoe that conforms to the shape of your foot. Opt for shoes with wider insteps, broad toes, and soft soles. Shoes that are short, tight, or sharply pointed should be avoided.
What Are The Key Reasons For Overpronation Of The Feet
The majority of the population have a normal to low arch. Even though the arches appear to be normal most of us suffer from over-pronation during walking, running and standing, due to the hard, flat unnatural surfaces we walk on, combined with wearing unsupportive footwear. With every step we take the arches flatten and the ankles roll inwards. Pronation itself is not wrong because we need to pronate and supinate as part of our natural gait cycle. Pronation (rolling in) acts as a shock-absorbing mechanism and supination (rolling out) helps to propel our feet forward. Over-pronation occurs when the foot pronates too deep and for too long, not allowing the foot to 'recover' and supinate. Over-pronation hampers our natural walking pattern. It causes an imbalance and leads to wear and tear in several parts of the body with every step we take.

Causes
There has been some speculation as to whether arch height has an effect on pronation. After conducting a study at the Rose-Hulman Institute of Technology, Maggie Boozer suggests that people with higher arches tend to pronate to a greater degree. However, the generally accepted view by professionals is that the most pronation is present in those with lower arch heights. To complicate matters, one study done by Hylton Menz at the University of Western Sydney-Macarthur suggests that the methods for measuring arch height and determining whether someone is ?flat-footed? or ?high-arched? are unreliable. He says, ?For this reason, studies investigating the relationship between static arch height motion of the rearfoot have consistently found that such a classification system is a poor predictor of dynamic rearfoot function.
Symptoms
It is important to note that pronation is not wrong or bad for you. In fact, our feet need to pronate and supinate to achieve proper gait. Pronation (rolling inwards) absorbs shock and supination (rolling outwards) propels our feet forward. It is our body?s natural shock-absorbing mechanism. The problem is over-pronation i.e. the pronation movement goes too deep and lasts for too long, which hinders the foot from recovering and supinating. With every step, excess pronation impedes your natural walking pattern, causing an imbalance in the body and consequent excessive wear and tear in joints, muscles and ligaments. Some common complaints associated with over-pronation include Heel Pain (Plantar Fasciitis) ,Ball of foot pain, Achilles Tendonitis, Shin splints, Knee Pain, Lower Back Pain.
Diagnosis
So, how can you tell if you have overpronation, or abnormal motion in your feet, and what plantar fasciitis treatment will work to correct it? Look at your feet. While standing, do you clearly see the arch on the inside of your foot? If not, and if the innermost part of your sole touches the floor, then your feet are overpronated. Look at your (running/walking) shoes. If your shoes are more worn on the inside of the sole in particular, then pronation may be a problem for you. Use the wet foot test. Wet your feet and walk along a section of pavement, then look at the footprints you leave behind. A normal foot will leave a print of the heel connected to the forefoot by a strip approximately half the width of the foot on the outside of the sole. If you?re feet are pronated there may be little distinction between the rear and forefoot.

Non Surgical Treatment
One of the best forms of treatment for over pronation is wearing supportive shoes. Shoes should have ample support and cushioning, particularly through the heel and arch of the foot. Without proper shoes, there may be additional strain on the tissue in the foot, greatly contributing to or causing an occurrence of over pronation. Rarely is surgery considered to relieve the pain and damage that may have resulted from this condition. Orthotic shoe inserts are often the easiest and most effective way to correct pronation.
Prevention
Wearing the proper footwear plays a key role as a natural way to help pronation. Pronated feet need shoes that fit well, provide stability, contain supportive cushioning, are comfortable and allow enough room for your foot to move without causing pain or discomfort. Putting special inner heel wedges, known as orthotics, into your shoes can support a flatfoot while lowering risks of developing tendinitis, according to the American Academy of Orthopaedic Surgeons. More extensive cases may require specially fitted orthopaedic shoes that support the arches.
Will Severs Disease Necessitate Surgery Treatment?
Sever?s disease, or calcaneal apophysitis, is a common cause of heel pain in patients whose bones are still growing; however, it is not really a disease. The pain is caused by stress at the point where the Achilles tendon meets tissue called the plantar fascia on the growth plate (apophysis) of the heel bone (calcaneus).
Sever's affects boys more often than girls. Boys are most often affected at age 12, and girls at age 9, though Sever's is typically seen in children and adolescents between the ages of 7 and 15.
Causes
Physically active children run the risk of developing Sever?s disease because they put the most strain on their growing bones. Sever?s usually occurs during the adolescent growth spurt, when young people grow most rapidly. (This growth spurt can begin any time between the ages of 8 and 13 for girls and 10 and 15 for boys.) By age 15 the back of the heel usually finished growing. As teens grow, the growth plates harden and the growing bones fuse together into mature bone. Young people engaged in physical activities and sports that involve jumping and running on hard surfaces-such as track, basketball, soccer, and gymnastics-are ata higher risk for developing Sever?s disease. Poor-fitting shoes can contribute by not providing enough support or padding for the feet or by rubbing against the back of the heel.
Symptoms
The most common symptoms of Sever?s involves pain or tenderness in one or both heels. This pain usually occurs at the back of the heel, but can also extend to the sides and bottom of the heel. A child with Sever?s may also have these common problems. Heel pain with limping, especially after running. Difficulty walking. Discomfort or stiffness in the feet upon awaking. Swelling and redness in the heel. Symptoms are usually worse during or after activity and get better with rest.
Diagnosis
A doctor can usually tell that a child has Sever's disease based on the symptoms reported. To confirm the diagnosis, the doctor will probably examine the heels and ask about the child's activity level and participation in sports. The doctor might also use the squeeze test, squeezing the back part of the heel from both sides at the same time to see if doing so causes pain. The doctor might also ask the child to stand on tiptoes to see if that position causes pain. Although imaging tests such as X-rays generally are not that helpful in diagnosing Sever's disease, some doctors order them to rule out other problems, such as fractures. Sever's disease cannot be seen on an X-ray.
Non Surgical Treatment
Treatment revolves around decreasing activity. Usual treatment has been putting children in a boot in slight equinus, or a cast with the foot in slight equinus, thereby decreasing the tension on the heel cord, which in turn pulls on the growth plate at the heel. As the pain resolves, children are allowed to go back to full activities. Complete resolution may be delayed until growth of the foot is complete (when the growth plate fuses to the rest of the bone of the heel). A soft cushioning heel raise is really important (this reduces the pull from the calf muscles on the growth plate and increases the shock absorption, so the growth plate is not knocked around as much). The use of an ice pack after activity for 20mins is often useful for calcaneal apophysitis, this should be repeated 2 to 3 times a day. As a pronated foot is common in children with this problem, a discussion regarding the use of long term foot orthotics may be important. If the symptoms are bad enough and are not responding to these measures, medication to help with inflammation may be needed. In some cases the lower limb may need to be put in a cast for 2-6 weeks to give it a good chance to heal.
Surgical Treatment
The surgeon may select one or more of the following options to treat calcaneal apophysitis. Reduce activity. The child needs to reduce or stop any activity that causes pain. Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue. Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile. Often heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis, or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.
What Is Posterior Tibial Tendon Dysfunction ?
Overview
Over 60 Million Americans suffer from Adult Acquired Flatfoot (AAF), otherwise known as Posterior Tibial Tendon Dysfunction or PTTD. This condition generally occurs in adults from 40-65 years of age, and it usually only occurs in one foot, not both. The Posterior Tibial (PT) Tendon courses along the inside part of the ankle and underneath the arch of the foot. It is the major supporting structure for the arch. Over time, the tendon becomes diseased, from overuse, and starts to lose it's strength. As a result, the arch begins to collapse, placing further strain on the PT Tendon, leading to further decrease in tendon strength, which causes further collapse of the arch. This is described as a progressive deformity because it will generally get worse over time. 
Causes
Women are affected by Adult Acquired Flatfoot four times more frequently than men. Adult Flatfoot generally occurs in middle to older age people. Most people who acquire the condition already have flat feet. One arch begins to flatten more, then pain and swelling develop on the inside of the ankle. This condition generally affects only one foot. It is unclear why women are affected more often than men. But factors that may increase your risk of Adult Flatfoot include diabetes, hypertension, and obesity.
Symptoms
In many cases, adult flatfoot causes no pain or problems. In others, pain may be severe. Many people experience aching pain in the heel and arch and swelling along the inner side of the foot.
Diagnosis
The diagnosis of tibialis posterior dysfunction is essentially clinical. However, plain radiographs of the foot and ankle are useful for assessing the degree of deformity and to confirm the presence or absence of degenerative changes in the subtalar and ankle articulations. The radiographs are also useful to exclude other causes of an acquired flatfoot deformity. The most useful radiographs are bilateral anteroposterior and lateral radiographs of the foot and a mortise (true anteroposterior) view of the ankle. All radiographs should be done with the patient standing. In most cases we see no role for magnetic resonance imaging or ultrasonography, as the diagnosis can be made clinically.
Non surgical Treatment
Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In many cases of PTTD, treatment can begin with non-surgical approaches that may include orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe. Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weight-bearing for a while. Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may advise changes to make with your shoes and may provide special inserts designed to improve arch support. 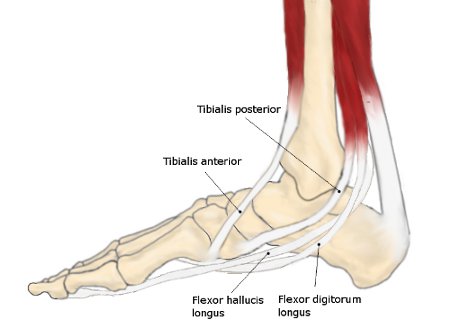
Surgical Treatment
If cast immobilization fails, surgery is the next alternative. Treatment goals include eliminating pain, halting deformity progression and improving mobility. Subtalar Arthroereisis, 15 minute outpatient procedure, may correct flexible flatfoot deformity (hyperpronation). The procedure involves placing an implant under the ankle joint (sinus tarsi) to prevent abnormal motion. Very little recovery time is required and it is completely reversible if necessary. Ask your Dallas foot doctor for more information about this exciting treatment possibility.
Will Adult Aquired Flat Foot Necessitate Surgical Teatment ?
Originally known as posterior tibial tendon dysfunction or insufficiency, adult-acquired flatfoot deformity encompasses a wide range of deformities. These deformities vary in location, severity, and rate of progression. Establishing a diagnosis as early as possible is one of the most important factors in treatment. Prompt early, aggressive nonsurgical management is important. A patient in whom such treatment fails should strongly consider surgical correction to avoid worsening of the deformity. In all four stages of deformity, the goal of surgery is to achieve proper alignment and maintain as much flexibility as possible in the foot and ankle complex. However, controversy remains as to how to manage flexible deformities, especially those that are severe.

Causes
There are numerous causes of acquired Adult Flatfoot, including, trauma, fracture, dislocation, tendon rupture/partial rupture or inflammation of the tendons, tarsal coalition, arthritis, neuroarthropathy and neurologic weakness. The most common cause of acquired Adult Flatfoot is due to overuse of a tendon on the inside of the ankle called the posterior tibial tendon. This is classed as - posterior tibial tendon dysfunction. What are the causes of Adult Acquired flat foot? Trauma, Fracture or dislocation. Tendon rupture, partial tear or inflammation. Tarsal Coalition. Arthritis. Neuroarthropathy. Neurological weakness.
Symptoms
Symptoms of pain may have developed gradually as result of overuse or they may be traced to one minor injury. Typically, the pain localizes to the inside (medial) aspect of the ankle, under the medial malleolus. However, some patients will also experience pain over the outside (lateral) aspect of the hindfoot because of the displacement of the calcaneus impinging with the lateral malleolus. This usually occurs later in the course of the condition. Patients may walk with a limp or in advanced cases be disabled due to pain. They may also have noticed worsening of their flatfoot deformity.
Diagnosis
The diagnosis of posterior tibial tendon dysfunction and AAFD is usually made from a combination of symptoms, physical exam and x-ray imaging. The location of pain, shape of the foot, flexibility of the hindfoot joints and gait all may help your physician make the diagnosis and also assess how advanced the problem is.
Non surgical Treatment
There are many non-surgical options for the flatfoot. Orthotics, non-custom braces, shoe gear changes and custom braces are all options for treatment. A course of physical therapy may be prescribed if tendon inflammation is part of the problem. Many people are successfully treated with non-surgical alternatives.

Surgical Treatment
A new type of surgery has been developed in which surgeons can re-construct the flat foot deformity and also the deltoid ligament using a tendon called the peroneus longus. A person is able to function fully without use of the peroneus longus but they can also be taken from deceased donors if needed. The new surgery was performed on four men and one woman. An improved alignment of the ankle was still evident nine years later, and all had good mobility 8 to 10 years after the surgery. None had developed arthritis.